It only took less than a week for the US to record more than 1 million Covid-19 cases. One expert says the disease is spreading ‘faster’ and ‘broader’ than ever.
At least 12,019,960 cases have been confirmed, according to Johns Hopkins University data, and 255,414 Americans have died.
On Friday, more than 195,500 new infections were reported — the country’s highest for a single day, and far beyond what the nation was seeing just weeks ago. The highest number of single-day cases during the country’s summer surge was a little more than 77,100 in July, Johns Hopkins University data shows.
Many are traveling for Thanksgiving despite CDC’s recommendation against it
“This is faster. It’s broader. And what worries me, it could be longer,” she said.
“I would say to those who are homesick…just hold the line,” Dr. Chris Pernell, a public health physician at New Jersey’s Newark University Hospital, told CNN on Saturday. “Hold on a little bit longer until we can get to the point in the nation where we know that the pandemic isn’t accelerating. Otherwise it could be deadly.”
Several people at Washington’s Reagan National Airport told CNN this week that they felt safe enough to fly.
“I understand the risk that I’m taking, but I want to see my family,” Yasmine Dehghani, who was flying to Connecticut, said.
Health experts, however, stress a negative test result will not guarantee a person isn’t carrying the virus to a Thanksgiving gathering, because a test won’t necessarily pick up on fresh infections. An already-infected person could test negative, travel to a dinner days later and then spread the disease.
What rising cases and hospitalizations mean for the country
The rising numbers have brought some hospital systems to their knees and prompted state leaders to take action to help curb the spread.
At least 24 hospital leaders warned the American Hospital Association they are experiencing staffing shortages, Nancy Foster, the association’s vice president for quality and patient safety policy, said. Those concerns have been raised in states including Texas, Wisconsin, Illinois, Minnesota and North and South Dakota, all of which have recently seen infections climbing, she added.
And those shortages are hard to fix when pulling from a workforce of health care employees “justifiably experiencing a significant emotional and physical toll due to the impact of the pandemic,” Foster said in a statement to CNN.
And in rural parts of the country, the challenge is often greater.
Of about 2,000 hospitals considered to be rural, about 1,700 have 50 beds or fewer and about 1,300 of them have 25 beds or fewer, according to Tom Morris, associate administrator for rural health policy in the federal government’s Health Resources and Services Administration.
“We’re not talking about large facilities. We’re not talking about a lot of ICU capacity,” Morris said during the National Institutes of Health rural health seminar.” In a lot of these hospitals, they’re able to offer an ICU of one of two beds.”
Responding to the crisis, multiple governors this week announced new measures to combat the surging infections and relieve strained hospital systems.
There is good news, too
Those include wearing a mask, social distancing, avoiding crowds and washing hands regularly. The University of Washington’s Institute for Health Metrics and Evaluation projected this week about 65,000 lives could be saved by March 1 if 95% of Americans wore masks.
The CDC and the Kansas Department of Health and Environment looked at case trends the month before the mandate and for the month after the mandate and found that in the 24 counties that required people to wear masks in public, there was a net decrease of 6% in cases. Meanwhile, in counties without the mandate, the disease continued to surge, with a net increase in cases of about 100%.
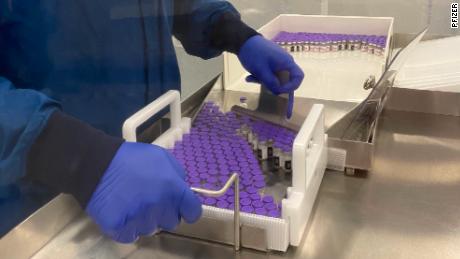
And soon, there could be more reinforcements in the battle against Covid-19.
While the application for EUA is “encouraging,” the Infectious Diseases Society of America stressed Friday that a transparent review of Pfizer’s data is still needed.
And if the vaccine is given the green light, “clinical trials and data collection must continue,” Dr. Barbara Alexander, president of IDSA, said in the statement.
“Measures that include wearing masks, frequent hand washing, maintaining physical distance and restricting the size of gatherings will remain crucial,” the statement said. “Finally, new federal funding must be provided for widespread, fair and equitable vaccine distribution in addition to campaigns to build vaccine confidence.”
CNN’s Michael Nedelman, Jason Hanna, Pete Muntean, Andy Rose, Jen Christensen, Jacqueline Howard, Maggie Fox and Hollie Silverman contributed to this report.
![]()