London’s hospitals will be overwhelmed by Covid patients in TWO weeks, stark NHS briefing warns
London’s hospitals will be overwhelmed by Covid patients in TWO weeks in a BEST CASE scenario with 2,000 beds needed even after Nightingale is opened, stark NHS briefing warns
- London hospitals will be overwhelmed in less than two weeks, report warns
- Medical director at NHS England London provided the worrying analysis
- Even if the number of coronavirus patients grew at the lowest likely rate and capacity is increased, the NHS would still be short 2,000 beds, it was claimed
London’s hospitals will be overwhelmed by Covid in less than two weeks even in a ‘best’ case scenario, an official briefing reportedly warns.
Vin Diwakar, medical director at NHS England London, provided the worrying analysis to medical directors of the capital’s hospital trusts over a Zoom call this afternoon.
Even if the number of coronavirus patients grew at the lowest likely rate and capacity is increased, including opening London’s Nightingale hospital, the NHS would still be short 2,000 general and acute and intensive care beds by January 19, the HSJ reports.
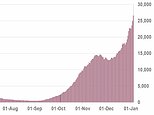
Three scenarios are laid out for both G&A and intensive care – ‘best’, ‘average’ and ‘worse’. These account for the impact of four per cent daily growth, five per cent growth and six per cent growth respectively.
Growth for G&A beds on January 5 was 3.5 per cent, with the rate at 4.8 per cent for ICU beds, reports claim.




The ‘best’ case forecast would mean the number of Covid patients in G&A beds rising to 9,500 by January 19, with non-Covid patients remaining the same at 7,460 – a number which remains constant throughout all the scenarios.
After small demand control measures, the total demand is predicted to be at 17,100.
Possible ways of increasing capacity includes the NHS securing an additional 400 beds, with the independent sector finding 50.
In addition to this, 1,000 ‘step down beds’, some supplied by the Nightingale hospital’s opening, and 150 made available by specialist trusts, would give a total capacity of 15,600 – still 1,500 short of the forecast demand.
The ‘average’ scenario would see a shortfall of 2,900 beds, with 4,400 in the ‘worse’ scenario.
The news comes as shocking footage from an intensive care unit revealed the extent of the coronavirus crisis and the strain it is piling on the NHS .
Emotional doctors and nurses were seen struggling at London ‘s University College Hospital while caring for the growing amount of coronavirus patients.
Operating theatres and some paediatric rooms have even been converted into intensive care units to deal with the ever-growing number of patients.


Emotional doctors and nurses were seen struggling at London’s University College Hospital while caring for the growing amount of coronavirus patients


The harrowing footage comes on the same day Britain breached 1,000 Covid-related deaths since the virus’s peak in April.
Department of Health figures revealed that a whopping 1,041 people have died as a result of coronavirus in the past 24 hours.
Footage filmed by the BBC showed the alarming reality on hospital wards.
One patient, Attila, 67, opened up about the trauma of suffering from the virus.
He said: ‘It knocked me out. I didn’t think I would make it. There is no oxygen around. It’s very frightening.’
A doctor went on to explain that if the hospital is forced to keep increasing its capacity at this rate it will only be able to last another week before it cannot provide intensive health care to all patients.
It comes after it was revealed that doctors may have to decide which severely ill patients to treat based on a ‘lottery’ if the NHS is overwhelmed this winter under draft Covid rationing plans.






Even if the number of coronavirus patients grew at the lowest likely rate and capacity is increased, including opening London’s Nightingale hospital, the NHS would still be short 2,000 general and acute and intensive care beds by January 19, the HSJ reports (stock image)
New guidance also advises medics look at patients’ potential to contribute to society or their likelihood of surviving the treatment as a way to prioritise whose lives should be saved.
The protocol says that for patients who are in similar health and cannot be separated in other ways, a ‘random allocation, such as a lottery, may be used’.
The document, published in the Journal for Medical Ethics in November, was drawn up by experts at a major NHS Trust in Bath in an attempt to come up with a system for rationing care in the event there are not enough resources to treat everyone.
It being widely circulated among NHS specialists, according to the Telegraph, as some trusts struggle to deal with a tsunami of coronavirus patients with the new, highly infectious strain of the disease.
Medical, legal and palliative care specialists at the Royal United Hospital Bath NHS Trust (RUHBT), who drafted the protocol, stressed the health service has not yet reached the tipping point at which care needs to be rationed.
Numerous hospital workers are needed to care for just one coronavirus patient that is on a ventilator.
Nine members of staff are needed to flip ventilator patients twice a day in order to help improve their airflow.
And hospital workers are not only bearing the physical brunt of the coronavirus crisis.
Many have been left emotionally drained by the appalling things they have seen.
One nurse said: ‘My emotions are all over the place. I’m scared, sad and worried.’
Another nurse, Ashleigh, revealed that they are being forced to prioritise their care which will inevitably lead to a lower standard of care.
The BBC’s medical editor, Fergus Walsh, said: ‘The staff are sell shocked. I saw staff in there in tears.’
He also revealed that there are currently 30,000 Covid patients in hospitals across the country – 9,000 more than at the virus’s peak in April.
And although the average age of a coronavirus patient in intensive care is 60, Mr Walsh revealed that there were patients in their 20s who are being treated in ICU at University College Hospital.
He added that doctors are eager to let the public know that urgent care is still available and if you are worried about ‘lumps and bumps’ or suffer a heart attack or stroke you should still be going to hospital so more lives are not lost unnecessarily.
![]()